https://sparkatncis.wordpress.com/2015/02/03/issue-4-a-dish-of-hope/#more-129
Issue 4 – A Dish of Hope
Ask any Singaporean about the best part of Singapore and their answer would be the same – her food.
Known far and wide for her culturally diverse mix of food bound to whet
just about anyone’s appetite, it is hard to resist the tantalising
spread of food across Singapore, which is no wonder why some would go
the distance by travelling from the East to the West and vice versa,
just to satisfy their food cravings.
Meet Yvonne, otherwise also known as a foodie,
defined as someone who has an ardent interest in food and seeks out
food experiences as a hobby. In the flesh, one would never think of
Yvonne as a foodie; petite and unreflective of a person with a voracious
appetite, Yvonne pleasantly surprised us with her love for food.
However, life for Yvonne has not always been peachy and her story is testament to not taking the littlest things such as eating, for granted.
Lost Childhood

Yvonne, as a young girl pictured with her grandmother
Her primary caregiver growing up 42 years old this year, Yvonne’s troubles began when she was just a
young girl. Growing up sandwiched between her parents’ tumultuous
marriage, Yvonne bore the brunt of a fruitless marriage when her parents
finally decided to divorce. The youngest child in the family, Yvonne
was cast to her grandmother, while her mother continued to care for both
her elder sister and brother. Isolated and neglected from her parents’
love, Yvonne found love and refuge under her grandmother’s wings who
took it upon herself to care and provide for her till adulthood.
A child estranged from her parents, Yvonne’s childhood was peppered
with troughs. When both her parents remarried, she once again found
herself caught between two separate families, with little emotional and
physical attachment to either. It was as though she was the missing
piece to the puzzle; even though she belonged somehow, but was
ultimately still lost without any sense of belonging.
The Rainbow after the Storm
When she was 21, Yvonne saw a glimmer of hope when she met the love
of her life, Eddie, through her cousin. In the blink of an eye, Eddie
and her now share a beautiful marriage of 21 years and counting, as well
as three lovely children, Gwen, Sean and Dawn, aged 20, 18 and 13 years
old respectively.
A victim of divorce, Yvonne fully understands the importance of
family and treasures every single moment spent with her family. She
brightens up as she tells us of her family’s love for bowling and of
course, their all-time favourite activity, eating! She giggles as she
referenced her husband to being the “jest of the family”, constantly
jostling the family into high spirits with his comical antics. Her voice
lowered into a note of seriousness as she expressed her heartfelt love
for her husband, and how thankful she was to have met him.
For the Love of Food
Yvonne then let us in on her favourite food haunts; a fan of local
food, Yvonne’s comfort food come in the form of ice-cream waffles,
chicken chop and steak, located at Kovan. She also delights in
Xiaolongbaos, a type of steamed bun that originates from the Jiangnan
region of China, found in Causeway Point shopping mall. Her eyes
sparkled as she enthusiastically added Serangoon and Marsiling to the
list, her favourite dishes there comprising of Hor Fun (a type of
Chinese noodles made of rice), crispy noodles, bitter gourd fish soup
and Wonton (dumpling) noodles.
A Twist of Fate
A trip down memory lane caused Yvonne’s lips to curl downwards as she
reminisced the time when food was not her friend. The year was 2011
when she discovered swollen lymph nodes on the left side of her neck; a
trip to her nearest General Practitioner diagnosed her with a bacterial
infection to be treated with antibiotics. However, the swelling never
subsided and one year later, to her horror, she discovered that the
lymph nodes on the right side of her neck were swollen too.
A delve into her family history uncovered her family’s run-in with
cancer; her mother was a victim of cervical cancer, and her sister, a
victim of throat cancer which she eventually succumbed to at age 40.
Yvonne was then scheduled for a blood test.
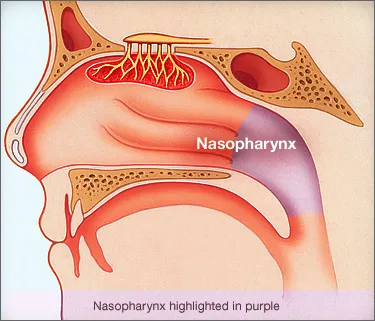
20 April 2012 – A date that remains permanently etched in Yvonne’s
mind as it was the day Yvonne found herself diagnosed with
Nasopharyngeal Cancer (NPC). Her world came crashing down as a biopsy
revealed her to be suffering from Stage 4 NPC, a large tumour located
behind the left side of her nose.
Tsunami of Bad News
Upon hearing the news, Yvonne found herself in the shoes of a young
girl she once filled years ago, lost and scared. However, this time
round, she was not alone. Her husband and friends were overwhelmed with
shock and sadness at the diagnosis and to Yvonne, it was as though the
happy life she built for herself was slowly crumbling away.
Another wave of bad news followed – Yvonne was told that she might
lose her sense of taste and was advised to extract all her wisdom teeth
before commencing on treatment. To someone whose life passion revolved
around food, the news came as a huge blow. Yvonne vividly recalled how
the news set her off on a food rampage to conquer all her favourite
foods to prepare for the worst case scenario.
The Route to Recovery
On 23 May 2012, Yvonne embarked on her chemotherapy treatment that
lasted over a period of four months. She shared with us her struggles as
an inpatient; with the treatments often leaving her drained, fatigued
and waned. Although dispirited, Yvonne kept her options open and never
lost hope, even participating in a research drug study that used novel
drugs aimed at shrinking tumourous growths in concurrence with
chemotherapy and radiation therapy treatment.
The course of treatment was very trying, said Yvonne as she suffered
from temporary hearing loss, blistered skin and an inability to swallow
food and drinks. However, she found comfort in her loved ones who
provided her with both emotional and physical support during this
period. No longer having to fight her battles alone, Yvonne’s family and
friends took turns to accompany her down for her treatment, a gesture
she is truly appreciative of.
Yvonne shared of how she drew strength from her doctors, as well as
the NPC Support Group, which she considers one of the biggest blessings
in her life.
To Yvonne, the NPC Support Group members are more than just beacons
of hope. Coming from all walks of life, battling and overcoming
different stages of cancer, their forthcoming passion and enthusiasm to
help others in the same boat has touched Yvonne’s heart and shaken its
core. To her, they are now her friends, her family, united in strength
and hope. It was with their support, that she got a better hold on what
to expect during her cancer journey, and how to cope.
After five cycles of chemotherapy and thirty-three sessions of
radiation therapy, Yvonne’s perseverance has paid off. Fast forward to
today and she has officially been declared cancer-free for two years
now. Yvonne believes she walked out of battle stronger than she ever
was, and has newfound joy, love and inner peace that have since shaped
her perception of life.
A Dish of Hope
A survivor who has emerged courageously from battle, Yvonne now has a
different take on life. To her, time is now tagged with a value, and
every moment has to be spent wisely, on things she holds dear to,
particularly spending time with her family and loved ones.
Apart from bowling and eating, Yvonne has also acquired a myriad of
new hobbies under her belt, ranging from singing, swimming, zumba to
yoga, healthy exercises that are beneficial to her health and personal
wellbeing.
Still an active member of the NPC Support Group, the once introverted
Yvonne has now broken out of her shell and relishes every opportunity
to inspire and motivate others around her, to fight arm in arm with
fellow cancer patients. She no longer lives life in the fast lane and
has learnt to slow down and not push herself too hard, be contented and
appreciate life to the fullest, let go of any misgivings and above all,
live life in moderation.
Battered but not broken, Yvonne wants others to know that life is an adventure, regardless of the circumstances one may be in. A strong heart and mind is the recipe to beating the disease and the journey to recovery will reward you with strength, inspiration and hope.

























.jpg)
.jpg)


.JPG)